How might we create a digital experience that enables large-scale, accurate health data collection without compromising trust, dignity, or access to care?
The answer didn’t arrive fully formed.
This project unfolded across multiple iterations, each shaped by what we observed in the field, beyond what had been scoped.
We started by:
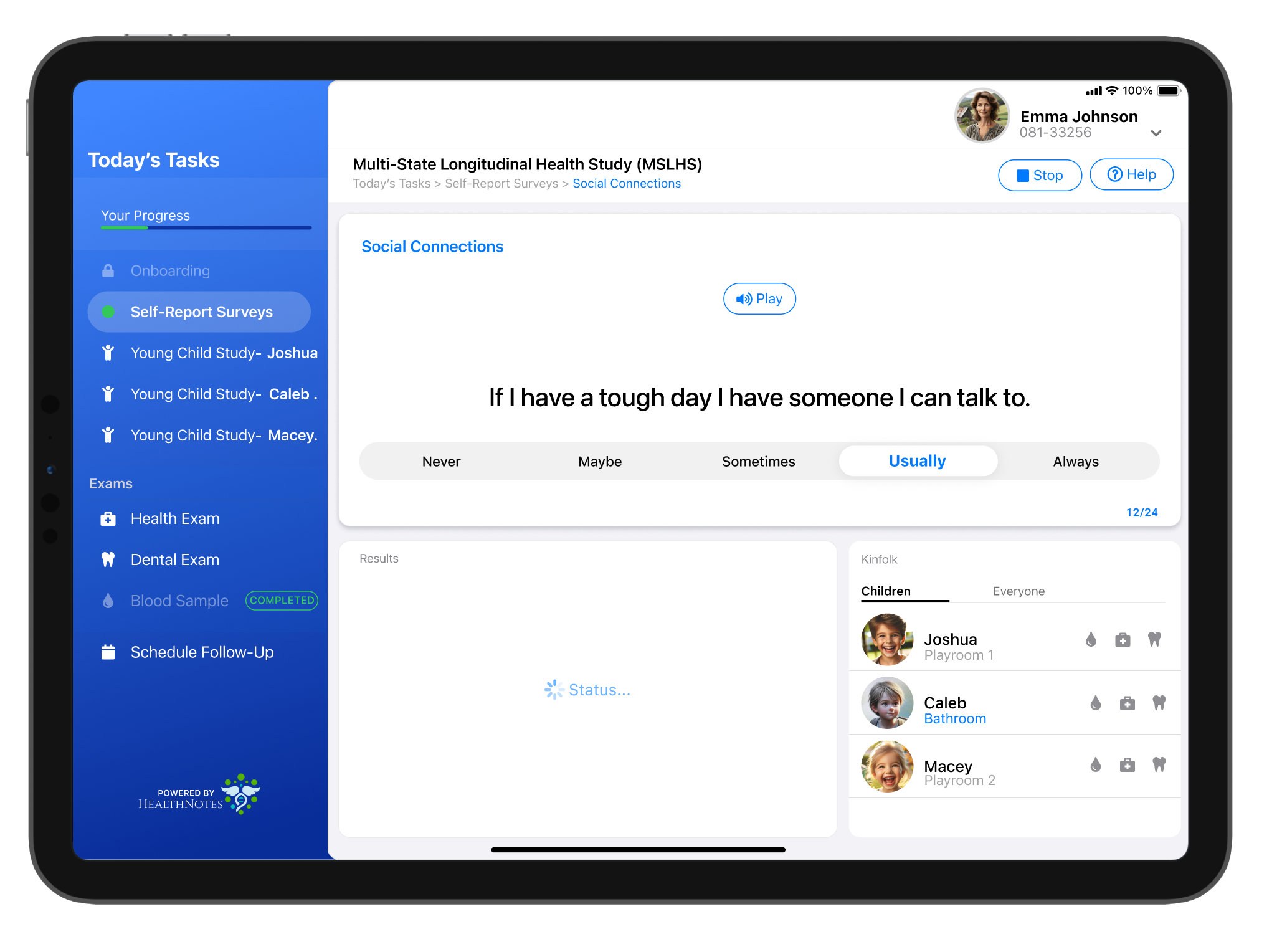
- Replacing paper surveys with a digital tablet flow
- Enabling speech guidance for users with low literacy
- Designing for offline data capture and fast transfer
Then, as we embedded in clinic environments, new problems surfaced:
- Clinicians were hand-drawing complex family trees—causing massive delays
- Patients were waiting all day and still leaving without care due to overflow emergencies
We adjusted course every time, expanding our design scope beyond UI into service delivery, trust repair, and systemic change.
.svg)